
Diabetes is believed to develop in those who eat a lot of sweets. In fact, it is a much more complex pathology, which only partly depends on diet and which can develop in any person.
Diabetes mellitus: definition of the disease
Diabetes mellitus (DM) is a group of diseases associated with metabolic disorders. People with diabetes cannot digest carbohydrates properly. As a result, their glucose (blood sugar) concentration increases significantly.
Glucose is a type of sugar that is the body's main source of energy.
Excess glucose has a toxic effect and destroys the walls of blood vessels, nerve fibers and internal organs.
Diabetes mellitus develops for various reasons. Some types of diseases are genetic in origin, while others are linked to lifestyle or environmental factors.
The name of the disease was given by the ancient Greeks. Translated from Greek, διαβαίνω means "to pass through", which refers to the main symptom of diabetes mellitus, polyuria or frequent urination. For this reason, a person continually loses fluid and strives to replenish it by drinking as much water as possible.
However, this is not always the case. Some forms of diabetes can develop asymptomatically for a long time or manifest so mildly that a person doesn't even notice anything is wrong. And even with the typical course of the disease, many years often pass before excess glucose in the blood leads to the appearance of symptoms of the disease. Moreover, all this time the person is in a state of hyperglycemia, and at the time of diagnosis he already suffers from serious irreversible disorders of the kidneys, blood vessels, brain, peripheral nerves and retina.
The disease causes significant damage to the body. Left untreated, excess glucose can lead to worsening function of the kidneys, heart, and nerve cells. But such complications can be avoided. Modern doctors have enough effective drugs and techniques to treat diabetes.
Prevalence
In 2019, diabetes was the direct cause of 1. 5 million deaths worldwide. Moreover, in almost half of the cases, the disease proved fatal in people under 70 years old. The other half of the patients died from complications of the disease: kidney failure, heart and vascular damage.

Besides humans, animals also suffer from diabetes. For example, dogs and cats.
From 2000 to 2019, the mortality rate from diabetes increased by 3% in developed countries and by 13% in lower-middle-income countries. At the same time, the likelihood of death from complications of the disease among people aged 30 to 70 has decreased by 22% globally. This is believed to be due to improved diagnosis of diabetes and effective methods of early prevention of its complications.
Classification of diabetes
In our country we use the classification of diabetes mellitus approved by the World Health Organization in 1999.
Type I diabetes mellitus
In this type of disease, a person's pancreas produces little insulin, a hormone needed to transport glucose into cells. As a result, glucose entering the blood cannot be completely absorbed by cells, remains in the vessels, is transported to tissues and gradually destroys them.
Depending on the cause of pancreatic dysfunction, type I diabetes is divided into two subtypes: immune-mediated and idiopathic.
Immune-mediated diabetes mellitusthe result of autoimmune destruction of pancreatic cells, due to which the immune system mistakenly attacks its own healthy tissues. Diabetes usually begins during childhood or adolescence, but can develop in people of any age.
Immune-mediated diabetes is often associated with other autoimmune diseases, such as Graves' disease, Hashimoto's thyroiditis, Addison's disease, vitiligo, or pernicious anemia.

Type 1 diabetes mellitus most often develops in children and adolescents, although it can occur at any age.
Idiopathic diabetes mellitus.A rare variant of the disease. These patients do not have laboratory signs of autoimmune damage, but symptoms of absolute insulin deficiency are observed.
Type II diabetes mellitus
In this case, the pancreas produces enough insulin, but the cells are insensitive or resistant to it, so they cannot absorb the glucose and it accumulates in the blood.
According to the main cause, diabetes mellitus type II is divided into diabetes mellitus type II with predominant insulin resistance and relative insulin deficiency and diabetes mellitus type II with predominant impaired insulin secretion with orwithout insulin resistance.
Other specific types of diabetes
Other specific forms of the disease include pathologies with a pronounced genetic component, associated with infectious diseases or taking certain medications, among others.
Genetic defects in pancreatic β-cell functionthe types of diseases in the development of which a defective gene is clearly established.
Genetic defects in insulin actionthe development of pathology is associated with the peripheral action of insulin, which is disrupted due to mutations in the insulin receptor gene.
Diseases of the exocrine pancreas.For example, chronic pancreatitis and other inflammatory pathologies.
Endocrinopathiespathologies associated with excessive secretion of other hormones, such as acromegaly, Cushing's disease, hyperthyroidism.
Drug- or chemical-induced diabetes, can occur when taking active hormonal substances, α- and β-adrenergic agonists, psychoactive, diuretic and chemotherapeutic drugs.
Diabetes associated with infectious diseases.As a rule, the disease develops due to viral infections (pathogens: Coxsackie, rubella, Epstein Barr virus).
Unusual forms of immunologically mediated diabetes. For example, immobility and rigidity syndrome, systemic lupus erythematosus.
Other genetic syndromes, sometimes associated with diabetes.
Gestational diabetes mellitus
It appears for the first time during pregnancy and is characterized by a reduction in the sensitivity of cells to glucose. The disease is believed to develop due to a hormonal imbalance. After delivery, the condition returns to normal or may progress to type II diabetes.
Causes of diabetes
Diabetes mellitus develops for a variety of reasons, including genetic and autoimmune disorders, chronic pancreatic diseases, and dietary habits.
Common Causes of Diabetes:
- dysfunction of the immune system, due to which it attacks pancreatic cells;
- genetic disorders that impair tissue sensitivity to glucose, change the function of the pancreas, and reduce or completely stop the synthesis of insulin necessary for glucose absorption;
- viral infections Coxsackie viruses, rubella, Epstein Barr, retroviruses can penetrate the cells of the pancreas and destroy the organ;
- chronic diseases affecting the pancreas, cystic fibrosis, pancreatitis, hemochromatosis;
- endocrine diseases Cushing's syndrome, acromegaly;
- toxins (e. g. rodenticides, used to kill rodents, heavy metals, nitrates);
- eating habits, an excess of fats and simple carbohydrates in the diet can lead to obesity and a decrease in the sensitivity of cells to insulin;
- medicines, certain hormonal medicines (in particular glucocorticoids), certain medicines for the treatment of diseases of the heart and nervous system, B vitamin preparations (in case of excessive consumption).
Diabetes risk factors
Depending on the type of diabetes, the risk factors for the disease differ.
Risk factors for type I diabetes:
- heredity - the likelihood of getting sick is higher if blood relatives suffer from diabetes;
- Some viral infections (e. g. , rubella, infectious mononucleosis) can trigger an autoimmune reaction in the body, causing the immune system to attack pancreatic cells.

Excess weight does not cause type I diabetes, but it increases the risk of developing type II diabetes.
The most common risk factors for type II diabetes mellitus, which are not directly related to increased blood sugar levels: excess weight, sedentary lifestyle, pregnancy, etc.
During physical activity, glucose is actively broken down to produce energy; Substances provided by food as well as the body's fat reserves are used as substrate. With obesity, the volume and, accordingly, the surface area of fat membranes and other cells containing lipid inclusions increases, the relative density of insulin receptors per unit area decreases, as a result, the cells become lesssensitive to insulin and absorb glucose is worse.
Risk factors for type II diabetes mellitus:
- overweight and obesity;
- a sedentary lifestyle (without physical activity, glucose breaks down more slowly, so cells may become less sensitive to insulin);
- diabetes mellitus in blood relatives;
- age over 45;
- Prediabetes is a condition in which blood glucose levels remain at the upper limit of normal for a long time. Prediabetes is said to be present if the analysis shows values of 5. 6 to 6. 9 mmol/l;
- diabetes mellitus during pregnancy (gestational diabetes);
- birth of a child weighing more than 4 kg;
- depression;
- cardiovascular illnesses;
- high blood pressure (pressure above 140/90 mm Hg);
- high levels of "bad" high-density cholesterol (more than 0. 9 mmol/l) and triglycerides (more than 2. 82 mmol/l);
- polycystic ovary syndrome.
Diabetes Symptoms
Type I diabetes mellitus usually manifests itself with pronounced symptoms; other types of illness may develop unnoticed for a long time.
Common Symptoms of Diabetes:
- strong thirst;
- weakness;
- frequent urination;
- bedwetting in children who have never wet the bed before;
- sudden weight loss for no apparent reason;
- strong feeling of constant hunger;
- frequent urinary tract infections or fungal infections.
In addition, there are so-called secondary symptoms of diabetes mellitus, which appear in the later stages of the disease and signal complications.
Secondary symptoms of diabetes:
- itchy skin;
- nausea;
- to vomit;
- abdominal pain;
- dry mouth;
- muscular weakness;
- Blurred vision;
- poorly healed wounds;
- numbness of fingers or toes;
- acanthosis nigricans darkening of the skin of the neck, armpits, elbows and knees;
- pigmented spots of diabetic dermopathy with atrophy and peeling of the skin, located in the bends of the lower extremities, often appear due to poor healing of leg wounds;
- Diabetic pemphigus blisters on the lower limbs varying in size from a few millimeters to several centimeters. Occurs most often in elderly patients with long-term diabetes;
- headache;
- acetone smell from mouth.

Acanthosis nigricans, or darkening of the skin on the neck, knees, elbows and armpits, can be a sign of diabetes.
Complications of diabetes
Complications typically develop in patients with advanced diabetes mellitus and include retinopathy, nephropathy, and polyneuropathy.
Destruction of large vessels leads to atherosclerosis, myocardial infarction, stroke and encephalopathy.
Constantly monitoring blood sugar levels and taking medications to lower their levels can prevent or delay irreversible complications of diabetes.
In addition, the regeneration of small vessels is disrupted. For this reason, wounds on the body do not heal well. So, even a small cut can turn into a deep, purulent ulcer.
Diabetic coma
Diabetic coma is a complication of diabetes associated with too high or, conversely, low blood sugar levels.
Depending on the concentration of glucose in the blood, diabetic coma is divided into two types: hypoglycemic (associated with a decrease in sugar levels) and hyperglycemic (caused by an increase in its level).
Hypoglycemic comausually occurs in people with diabetes who are taking insulin therapy.
The cause of such a coma is excess insulin, which prevents the body from raising blood sugar to normal levels. This often occurs when the insulin dose is incorrectly calculated or the diet is disrupted, in which the amount of insulin administered does not correspond to the portion of carbohydrates from the food consumed.
Precursors of hypoglycemic coma:
- tremble in the body,
- chills,
- dizziness,
- nervousness or anxiety
- intense hunger
- nausea,
- blurry vision,
- heart rhythm disturbances.
"Rule 15" to stop hypoglycemia in diabetes:
If your "sugar" level is reduced, you should eat 15 g of fast carbohydrates (drink juice, take a glucose tablet) and measure your blood sugar after 15 minutes. If its level is low, consume another 15 g of fast carbohydrates. Repeat these steps until the sugar reaches at least 3. 9 mmol/l.
In rare cases, hypoglycemia can cause a person to faint. In such a situation, he needs an urgent injection of the hormone glucagon, which is carried out by a paramedic.
Some people mistakenly believe that a person in a hypoglycemic coma needs to have a sugary liquid poured into their mouth. However, this is not the case and results in asphyxiation (suffocation).
Hyperglycemic comaaccompanied by an acute lack of insulin, which can be caused by severe stress or an insufficient dose of insulin after meals.

Dangerous hyperglycemia is said to occur if blood sugar exceeds 13. 9 mmol/L.
Symptoms of high blood sugar:
- strong thirst
- frequent urination,
- extreme fatigue
- blurry vision,
- smell of acetone or fruity breath,
- nausea and vomiting,
- abdominal pain,
- Rapid breathing.
If such symptoms appear, you should sit down as soon as possible, ask others to call an ambulance, or call an ambulance yourself.
Diagnosis of diabetes mellitus
If a person has symptoms of increased blood sugar levels: constant thirst, frequent urination, general weakness, blurred vision, numbness in the limbs, you should consult a general practitioner as soon as possible.
But most often diabetes mellitus develops asymptomatically, so all people are recommended to undergo a screening test once a year to detect the disease at an early stage and prevent the development of complications.
Which doctor should I contact if I suspect diabetes mellitus?
Typically, people first turn to a general practitioner. If diabetes is suspected, he refers them to a specialized specialist who treats metabolic pathologies, an endocrinologist.
During the consultation, the doctor will conduct a survey and examination, and to confirm the diagnosis and determine the severity of diabetes, he will prescribe laboratory and instrumental tests.
Inspection
If diabetes is suspected, the doctor will clarify the medical history: cases of illness in blood relatives, chronic pathologies of the pancreas, lifestyle, recent infectious diseases.
No specific signs of diabetes can be detected during the examination.
During the examination, the doctor will also assess the condition of the skin: in case of diabetes mellitus, dark areas of acanthosis nigricans may appear on it. Additionally, a specialist can perform a rapid blood sugar test. Exceeding normal values is a reason for further examination.
Laboratory research methods
For diagnosis, a blood sugar test is prescribed. Its high level along with characteristic symptoms such as constant thirst, frequent urination and frequent infectious diseases are a clear sign of diabetes.
Blood sugar is measured using one of the following tests: fasting and postprandial blood sugar test, glycated hemoglobin (HbA1c) level, which reflects the average blood sugar level over the past 3 months.
An HbA1c level not exceeding 6. 0% (42 mmol/l) and a glucose level not exceeding 5. 5 mmol/l are considered normal.
To make an accurate diagnosis, the study is carried out at least twice on different days. If the results are ambiguous, a glucose tolerance test is performed, which helps identify impaired cellular sensitivity to glucose.
Additionally, your doctor may order additional tests to distinguish type 1 diabetes from type 2 diabetes: an autoantibody test and a urine ketone body test.
Antibodies are usually present in people with type I diabetes and in ketone bodies with type II diabetes.
To assess the sensitivity of cells to insulin, the doctor can prescribe a test to calculate the HOMA-IR index (Homeostasis model Assessment of insulin Resistance), which takes into account the level of glucose and insulin in the blood. .
If hereditary forms of diabetes are suspected, experts may recommend genetic testing to identify mutations associated with hereditary forms of diabetes mellitus and glucose intolerance.
Instrumental research methods
Instrumental examinations make it possible to identify complications of diabetes: damage to the retina, damage to the heart, blood vessels, kidneys and nerve conduction disorders.
An ultrasound of the internal organs is prescribed to assess the condition of the kidneys and pancreas. Additionally, the doctor may refer the patient for an ECG to detect cardiac abnormalities.
To diagnose visual problems, you will need to consult an ophthalmologist. During an eye exam, the doctor assesses the condition of the retina and examines the cornea using a slit lamp or ophthalmoscope.
Diabetes treatment
There is no cure for diabetes. Treatment aims to maintain acceptable blood sugar levels and prevent complications of the disease.
People with diabetes need to measure their blood sugar regularly, inject insulin for type 1 diabetes or take tablets for type 2 diabetes, or inject insulin to control their blood sugar.
To prevent complications of the disease, your doctor may recommend other medications. For example, medicines to control blood pressure, thin the blood and prevent cardiovascular disease, as well as medicines that lower blood cholesterol.
Blood Glucose Monitoring
To monitor blood sugar levels, both classic glucometers and modern continuous monitoring systems are used.
A glucometer is a device equipped with a fine needle. A person pricks their finger with it and draws blood onto a special test strip. The glucometer immediately displays the result.
Monitoring systems are sensors installed on the shoulder, stomach or leg. These sensors continuously monitor blood sugar levels. Data from the device is automatically downloaded to a special monitor or to an application on the phone. Such devices can report spikes in blood sugar, plot blood sugar curves over periods of time, send information to your doctor, and even make recommendations on emergency and routine measures and the need to change management tactics. treatment of diabetes.

Wearing the monitoring system does not hurt; it is not felt on the body.
Diabetes diet
There is no special diet for people with diabetes, but it is important for people with this diagnosis to count the amount of carbohydrates they eat each day and keep a food diary.
Carbohydrate counting
Carbohydrates affect blood sugar levels the most. It is therefore important for people with diabetes not to eliminate them, but to count them.
Carbohydrate counting forms the basis of the diet of diabetic people on insulin therapy. To do this, use the universal bread unit (XE) setting.
1To absorb such an amount of glucose, an insulin dose of 1. 4 units is required.
The amount of carbohydrates in the diet of a person with type I diabetes should not exceed an average of 17 bread units per day.
The amount of carbohydrates a person with diabetes can normally tolerate varies from person to person and depends on weight, level of physical activity, daily calorie needs and how the body metabolizes carbohydrates.
You can calculate the required amount of carbohydrates per day with a nutritionist or your doctor. After converting the carbohydrates you eat into bread units, your doctor will help you determine the amount of insulin needed to absorb the glucose. Over time, a person will learn to calculate on his own.
Additionally, there are other dietary recommendations for people with diabetes:
- limit the caloric intake of all overweight patients;
- minimize the content of fats (mainly of animal origin) and sugars in foods;
- eat carbohydrates mainly from vegetables, whole grains and dairy products;
- exclude or limit the consumption of alcoholic beverages (no more than 1 conventional unit for women and 2 conventional units for men per day).
Prediction and prevention of diabetes mellitus
Diabetes mellitus is a chronic disease that cannot be completely cured. But medications and healthier lifestyle changes help avoid complications and slow the progression of the disease.
Without treatment, the prognosis for diabetes mellitus is unfavorable: a person may die due to damage to the cardiovascular system.
Ways to Prevent Diabetes:
- regular physical activity;
- varied diet with sufficient fiber, protein, fat and carbohydrates;
- healthy weight control;
- reduce alcohol consumption;
- stop drinking alcohol and smoking.
Nutrition for the prevention of type II diabetes mellitus
An important element of preventing type II diabetes is a healthy and varied diet. The principle, or method, of the healthy plate was developed for this purpose.
The Healthy Plate method divides foods into five main groups: fruits and vegetables, slow-release carbohydrates, dairy, proteins and fats. You can combine these groups using a regular plate. Fruits and vegetables should make up a third or half. Slow down the carbs by a third or a little more. The remaining part is occupied by dairy products, a little more protein foods and a small part by fats.
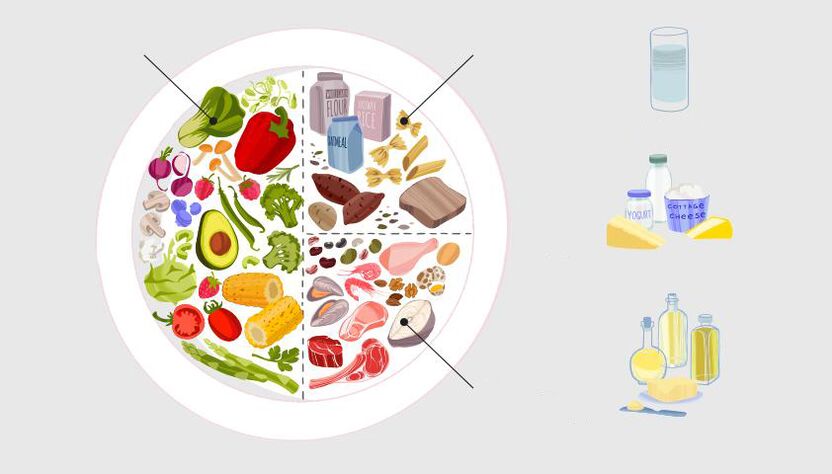
Eat according to the principle of a healthy plate: half consists of fiber, ⅓ of slow carbohydrates, the rest of protein foods.
In addition, other important principles of a healthy diet must be respected:
- drink according to thirst;
- eat less salt, no more than 1 teaspoon (5-6 g) per day;
- limit the consumption of trans fats (found in many fast food products, prepared and processed cakes and pastries);
- reduce the consumption of saturated fats (found in sweet pastries, fatty meats, sausages, butter and lard);
- eat less sugar, no more than 7 teaspoons (30 g) per day.
























